As many of you may know, I am a medical doctor by training and over the last ten years, I have been working as a scientist in a lab. The main goal of my work is to find new solutions for advancing care for cancer patients with metastatic disease. Often colleagues and students wonder why, after going through all that medical training, I decided to leave the “trenches” and work in a lab. So, I would like to share a piece of my story and my unconventional journey with you today while we discuss treatment options for metastatic breast cancer patients. I am a creative, action-oriented person; a problem solver some would say. Seeing the impact of my work on the well-being of patients has always been the most rewarding part of my job. I like to work with my brain and my hands to “fix” problems when they arise. So, after medical school, I started my surgical residency working with a multi-disciplinary group focusing on breast cancer patients.
It was quite rewarding to work with women that were diagnosed with early-stage breast cancers. We knew that by removing their tumors we would play a big role, along with oncologists and radiotherapists, in “fixing” the problem and in giving these women the opportunity to continue living a healthy life. However, our role as surgeons was very different when we were working with patients whose tumors had acquired the ability to colonize other organs like the lymph nodes, the bone, the lung, or the liver. Once tumors spread locally or systemically, removing these tumors through surgery is often not possible and other therapeutic options are conventionally used to treat these patients. So, could we somehow help the oncologists select the best therapeutic options for these patients?
When it comes to metastatic breast cancers, patients are usually treated with chemotherapy, targeted agents, or a combination of the two. But what is the difference between these types of treatments? Chemotherapy has historically represented the most utilized approach to treat metastatic cancer patients. Because cancer cells have a superior ability to grow and survive compared to normal cells, chemotherapies prevent cells from growing and dividing. However, these drugs are rather nonspecific and do not distinguish between dividing cancer and normal cells. Thus, normal cells are killed alongside cancer cells which causes unwanted side effects like hair loss, nausea, etc.
In the last two decades, the development of more sophisticated technologies has rapidly advanced cancer treatment as these new tools have allowed the scientific community to learn and understand more about the biology of cancers and the mechanisms that individual tumors rely on to survive. These discoveries have allowed us to understand that breast cancers cannot be considered as a single disease, but they are a collection of different diseases driven by distinct biological mechanisms. We have also realized that many of these survival mechanisms can be exploited and used as targets for developing new anti-cancer drugs. For example, some breast tumors have higher amounts of estrogen receptors compared to normal cells; they rely on estrogen for their growth. This biological observation has led to the development of drugs that prevent estrogen production or its interaction with the receptor. By interfering with these biological mechanisms, these new drugs have the ability to prevent the growth and survival of cancer cells. Every year the FDA approves new biological or targeted therapies designed to specifically interfere with molecules tumor cells utilize to thrive. Matching these drugs to the right patient is at the core of precision medicine.
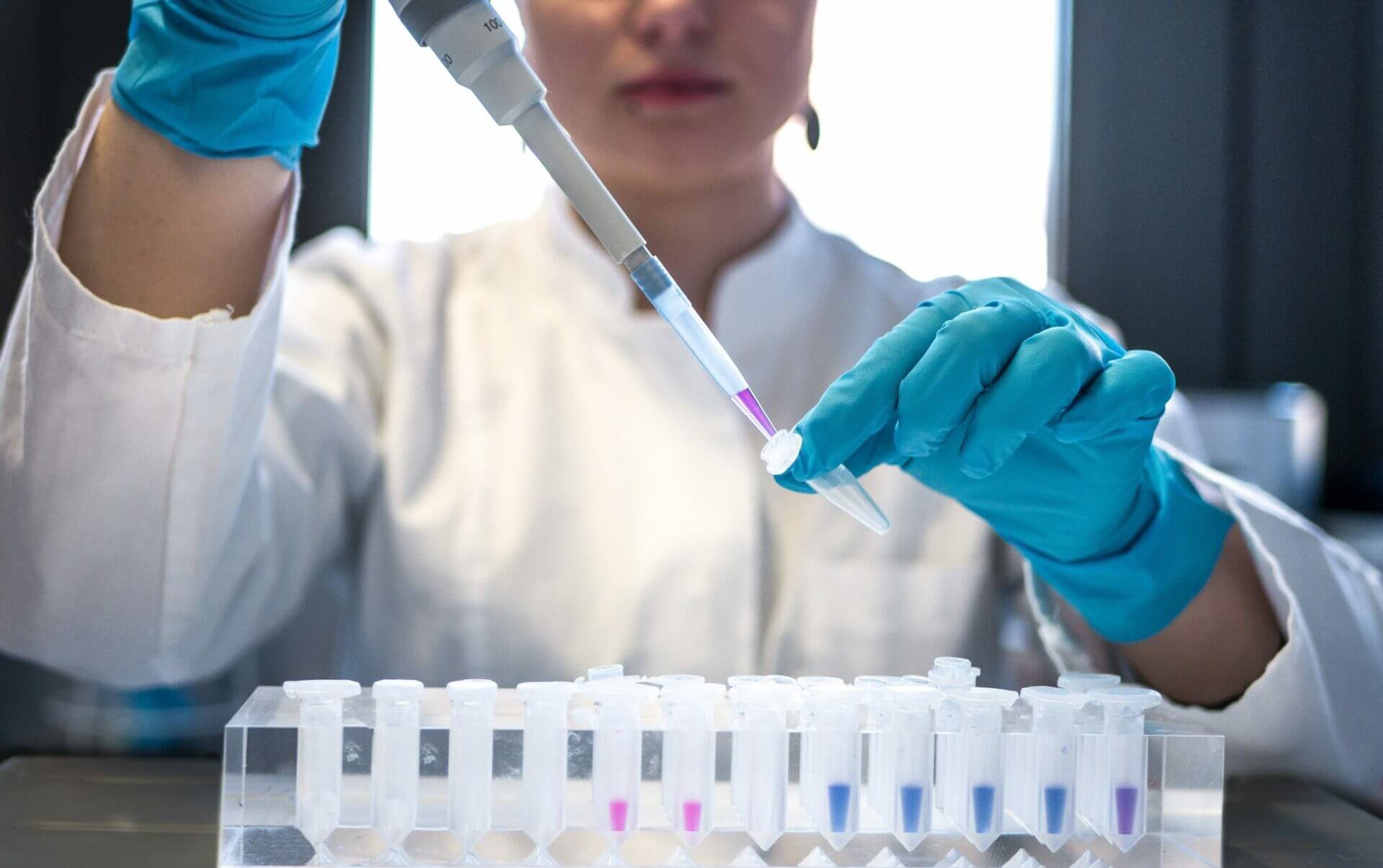
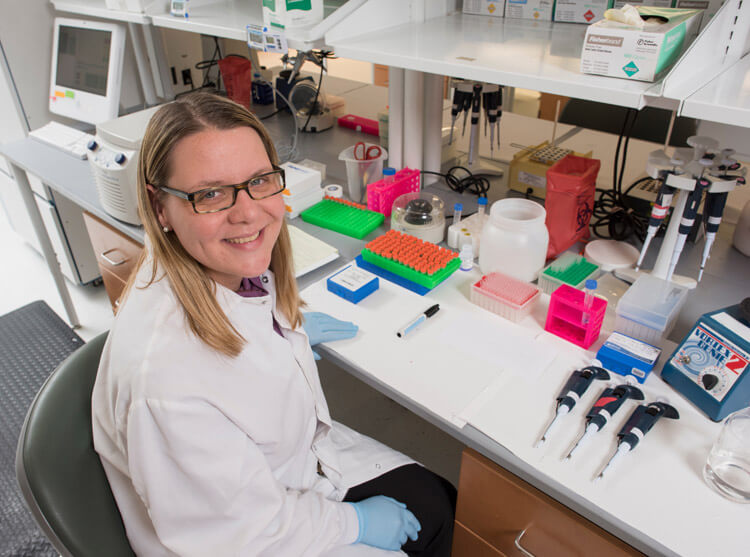
From a personal perspective, understanding that tumors can use such diverse mechanisms to grow and progress has brought me to realize that helping oncologists match each patient to the right drug is a key aspect for advancing treatments for patients with metastatic disease. And that can only be achieved in the lab. Using new technologies, we now have the ability to capture a glimpse of the mechanisms that drive individual tumors. These pictures are a much-needed guide for oncologists as they can be used to match a tumor’s biology with drug(s) that can interfere with driving mechanisms. Although there is still much to be learned about cancer biology and how to apply this knowledge to advance treatment for metastatic breast cancers, seeing patients matched to the right drug in our trials gives me hope that all our efforts, little by little, will make metastatic breast cancer a more manageable disease.